To anyone that uses drugs or cares for someone who does:
The drugs available in the UK seem to be changing lately. As services that provide support to people who use drugs and their loved ones, we have come together to issue a shared statement about some of the new drugs being used by the people we support and the risks they present.
Today is International Overdose Awareness Day, and in honour of all those who have been affected by overdose and in light of new information about synthetic opioids, we have updated our joint statement.
In the last two years, new opioids called “nitazenes” have arrived in the UK. They have recently been found mixed with heroin, with some being sold as illicit oxycodone pills and illicit ‘Xanax’ powders.
Nitazenes can be at least as strong as fentanyl and can be hundreds of times more potent than heroin. They are known to have led to accidental overdoses and the deaths of people across the UK in recent weeks.
If you use drugs, this information could help you and your friends to stay safer. If you know people who use drugs but do not use drugs yourself, the following information could help you to keep people alive.
Because of how dangerous these contaminated drugs are, the way you use drugs may need to change to avoid overdose. We have updated the following information, in line with harm reduction guidance issued by EuroNPUD, with additional information provided to aid those living in the UK:
1. Carry naloxone
- Always carry naloxone. It’s available from all drug services.
- If you live in Scotland: Scottish Families Affected by Alcohol and Drugs offers a ‘click & deliver’ service.
- If you live in Wales: Barod offers a ‘click & deliver’ service.
- Nitazenes have been found in non-opioid drugs (like illicit Xanax), so even if you or your friends don’t normally use opioids, it is still worth carrying naloxone.
- Carry extra naloxone – in some cases, it has taken multiple doses of naloxone to reverse overdoses involving heroin contaminated with synthetic opioids. Carry two yellow cases of intramuscular naloxone or two double packs of nasal naloxone. More advice is provided in point six (overdose response).
2. Don’t use alone
- Try not to use drugs alone, and don’t let your friends use them alone either. Watch out for signs of overdose in others. The signs include difficulty breathing, blue colouring to the lips or fingertips, unresponsiveness, and limp limbs.
- If you are going to use drugs, reach out to someone to let them know your plans and ask them to check up on you.
- If you are using with others, avoid all using at the same time. More advice on this is provided in point five (stagger your dose).
If you don’t have people to stay nearby or check on you, consider using the BuddyUp app.
3. Check your drugs
- Submit an anonymous sample of the substance to the WEDINOS Project for analysis. It will take a few days to get the results back, so go easy in the meantime.
- Fentanyl strips do not test for nitazene.
4. Start low, go slow
- Start with a lower dose and wait for the peak effects to pass.
- If you’re using illicit pills, consider splitting them and starting with a fraction of the pill. If you can’t split the pill, you might want to consider using the crush, dab, wait method. This was designed for MDMA users and is more applicable to powder or crystal form drugs, but could also keep you safer when using other pills.
5. Stagger your dose
- Make sure you are with a friend and one or both of you have naloxone.
- If one person takes their hit first, wait until the peak effects have worn off before the other person uses. This makes it much more likely that there is someone who can respond in the case of an overdose.
6. Overdose response
- If someone overdoses, administer naloxone and call an ambulance.
- Recent overdoses have required multiple doses of naloxone. You do not need to give doses at a faster rate, but you might need more than one naloxone kit. Continue to administer naloxone as you were trained to, and do not give multiple doses at once.
- Aim to restore breathing rather than consciousness. As well as synthetic opioids, drugs may be contaminated with other substances such as benzos or xylazine, which can lead to heavy sedation.
- Overdose symptoms returning is more likely with nitazenes, so make sure you observe someone for longer than you would with a normal heroin overdose.
- Naloxone only works on opioids. It’s best to use naloxone if you think someone has overdosed, even if you’re not sure what they’ve taken – naloxone will not harm them.
- While mixing different drugs is common, it is more likely to cause an overdose. Try to use one drug at a time. If you are going to mix drugs, use less of each.
7. Seek substitute medication and other prescribing support
- If you use opioids every day, your local drug service can support you and prescribe alternatives such as methadone or buprenorphine. Abstinence does not need to be your goal; these alternatives can help to keep you much safer.
- “The best way to reduce your chances of an overdose is to be on an opioid substitution treatment. Even if you are still taking drugs, if you are on methadone or buprenorphine, you are less likely to overdose, and you are less likely to die… If you are on a script, you are less likely to overdose and if you do, you are less likely to die” (Streve Brinksman, Cranstoun).
- The above quote is from a recent Cranstoun Tiktok. You can hear the rest of the message on TikTok.
- If you are already in treatment for opioid dependence and you don’t want to use on top, speak to your prescriber and make sure you’re getting the right dose for you.
- Check out the SODA tool to help you determine if your dose is right.
- If you do still want to use on top, that is okay too, but be aware that there are higher risks now of overdosing.
- If you don’t use opioids but are worried about your drug use and you take illicit benzos every day, you can also talk to your treatment provider about how they can support you.
Signed:
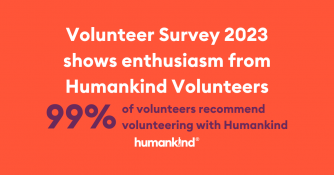
- Jon Findlay (National Harm Reduction Lead, Humankind)
- Deb Hussey (National Safer Lives Lead – Turning Point)
- Peter Furlong (National Harm Reduction Lead – Change Grow Live)
- Chris Rintoul (Innovation & Harm Reduction Lead – Cranstoun)
- Kate Blazey (Interim Medical Director – With You)
- Dr. Judith Yates (International Doctors for Healthier Drug Policies: IDHDP)
- Shayla S. Schlossenberg (Drugs Service Coordinator, Release)
- Mat Southwell (Project Executive, EuroNPUD)
- Roz Gittins (Director of Care Standards and Practice Improvement, Via)
- Rob Barker (Campaigns and Communications Lead, Barod)
- Justina Murray (CEO, Scottish Families Affected by Alcohol and Drugs)
- Prof Adam Winstock (Consultant psychiatrist & addiction medicine specialist)